1.0. INTRODUCTION
A health care system is the organization of people, institutions, and resources that deliver health care services to meet the health needs of target populations. The healthcare system in West Africa remained the worst in the world compared to the regions. Few countries in Sub-Saharan Africa are able to spend $34 to $40 a year per person for basic healthcare (World Health Organization). In addition, 50 percent of the region’s health expenditure is financed by out-of-pocket payments from individuals. However, it is estimated that $25-$30 billion would be needed in investing in the health care system in Africa (IFC, World Bank). Togo is located in West Africa and currently faces a healthcare crisis. According to Africa Development and Cooperation (2017), Togo was described as having the worst health systems in West Africa due to the persistent high morbidity and mortality rates in the country. However, insufficient staff, outdated medical instruments and practices, and ineffective financial and insurance resources remained the main factors that contribute to the sub-par healthcare systems in Togo.

Source: http:// www.who.int/countries/en/
1.0. HEALTHCARE SYSTEM IN TOGO
Under the reform by the Government of Togo, progress has been made under the Millennium Development Goals (MDG). In 2013, malaria was the leading cause of morbidity in all age groups (46%), and of mortality (12.26%) in health facilities. In 2010-2013, HIV prevalence fell from 3.2% to 2.5%, the number of new infections halved, whiles the rate of mother-to-child transmission fell from 34.9% to 14.7% significantly. Again, tuberculosis reduced from 77 to 58 cases per 100 000 of the population between the years 2005 and 2014. On the other hand, mortality increased from 10 to 13 deaths per 100 000 of the population in the country. In 2014, the TB/HIV coinfection rate remained high at an estimated 21%. Relating non-communicable diseases in Togo, there is higher exposure to risk factors such as tobacco use, alcohol abuse, the use of drugs and other psychoactive substances, and obesity. Due to that, ages from 15 to 64, the prevalence of high blood pressure is 19% and that of diabetes 2.6%. In addition, cardiovascular diseases are responsible for 6% of all deaths recorded at health-care facilities nationwide. On March 23, 2014, the World Health Organization (WHO) reported cases of Ebola Virus Disease (EVD) in the forested rural region of southeastern Guinea. The identification of these early cases marked the beginning of the West Africa Ebola epidemic, the largest in history and Togo actively prepared itself to address public health emergencies in the years 2014 and 2015. Recently, 67 suspected cholera cases presenting with diarrhea and vomiting, including two deaths a case fatality ratio (CFR: 3%) were recorded and a number of other cases reported in different cities.

Colin Petersdorf Photo: Flickr (2019). https://borgenproject.org/
1.0. HEALTH POLICIES AND SYSTEMS
Through the partnership with the International Health Partnership and related initiatives (IHP+) since 2010, Togo’s healthcare strategic framework system has been reformed. In May 2012, the Togolese government and its partners supported the implementation of the health development plan through planning and annual reviews at the operational and central levels of the health system. Moreover, there outlined the plans for the period 2012-2015 and a joint framework for monitoring and evaluation. Moreover, Togo’s health system is relatively well-equipped in terms of infrastructure, and 70.9% of the population have access to facilities even though geographical, economic, and social disparities regarding the supply and accessibility of essential health care persist.
In addition, the capital city has been concentrated by the distribution of human resources for health rural areas. Various initiatives are in place to improve the distribution of health workers and access to high-quality and affordable essential and generic medicines is inadequate due to the weak supply system.

© Childfund @ Togo: Investing in the Future: Health Care Programs in Togo
1.0. HEALTH FINANCING IN TOGO
In 2010, the Togolese government through the health reform created an evidence-based health plan, known as Compacts, which reflect enhance partnerships and dialogue within regional initiatives such as the Harmonization for Health in Africa (HHA) and the International Health Partnership (IHP+). In addition, Togo drafted a new National Health Policy and a National Health Development Plan in 2011 for the coming years in 2012- 2015. However, the health sector’s investment is low (approximately 5%) with low disbursement, and under mobilization of internal resources. The people in the country (almost half 51%) spend out-of-pocket expenditure by households for the direct payment system involving user fees, or cost recovery, and the purchase of medicines by patients. The government allocated a budget of 41% for cost recovery in 2006.
Again, other authorities such as the local authorities (town halls or prefectures) also finance health services by paying salaries to prefecture health workers through decentralization policy in the health service delivery system.
In addition, through external cooperation programs with the government and direct funding to grassroots communities, non-governmental organizations, and associations, the developmental partners provide financial supports to the health sector. On the other side, the political instability in the country between 1990 and 2005, there was a reduction (62%) in official development assistance and a reduction in the share of external assistance in the gross domestic product (GDP) from 13.8% to 3.3%.
Also, the European Union and international financial institutions through aid to an envelope of approximately US$20 to US$26 million per year. The World Health Organization Country Cooperation Strategy for Togo (2009-2013) has supported through several strategic priorities, such as health and community system strengthening, and identifies the drafting of a national strategy to finance and develop universal health coverage (UHC) as a strategic action.
Moreover, the health accounts for 2010, 2011, and 2012, now in preparation, only 7.6% of the population is covered by a system of financial risk protection. Again, only 4.4% of the population is covered by mandatory health insurance for public-sector workers. Initiatives are currently underway to extend protection to workers in the public, informal and agricultural sectors.
2.0. HEALTH FINANCING FUNCTIONS
2.1. Revenue contribution and collection:
The Togolese government is working on public financial management reforms with the International Monetary Fund and the World Bank to mitigate such fiduciary risks due to the irregular flow of funds from the government and external partners. Also, steady and sufficient resources are needed to ensure revenue forecasting and budget formulation. The state budget for the sector (6% on average of 2005 to 2008 national budget, Medium Term Expenditure Framework or MTEF, 2010- 2013) is far from meeting the commitment of 15% made through the Abuja Declaration. Further, the Ministry of Health has developed an MTEF that provides information on the sector’s financing requirements over the period of 2010-2013.
2.2. Pooling
The National Health Policy was introduced in 2009-2013 for the development of different solidarity mechanisms to extend health insurance and access to community-based health insurance, or mutuelles, and for better management of health subsidies. An estimated 6% of the population is covered by some type of health insurance. Social insurance programs in Togo include agencies that cover old-age pensions, disability, family allocations, and health insurance to workers in the public and formal private sectors.
Later, legislation calling for the establishment of a national health insurance scheme targeting civil servants, central administration staff, local collectivities, para-public agencies, and retired public sector workers was passed in 2011. The same year, fees for caesarian sections were waived. In 2012, the national health insurance scheme, (Institut National d’Assurance Maladie or INAM) began paying for the health services included in its benefits package, covering approximately 300,000 people as of 2016.
2.3. Purchasing:
To improve service quality, efficiency, and equity in the delivery of health service in Togo, there is an allocation of financial resources to providers, and health facilities and premiums and cost structures have been evaluated to ensure the financial sustainability of INAM and sufficient resource flow to health services, and provision of health services and the needs of the population.
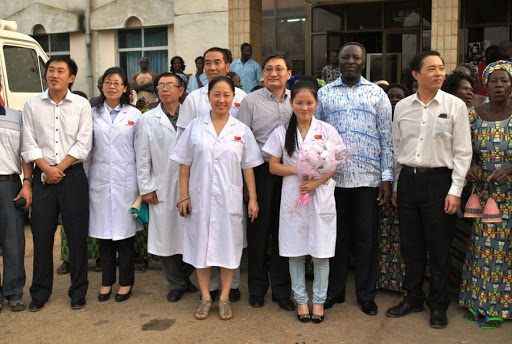
Chinese medical team provides free healthcare in southern Togo.
Source: www.xinhuanet.com
1.0. FUNDINGS OF HEALTH SECTOR IN THE MIDST COVID-19
The World Bank Group, one of the largest sources of funding and knowledge for developing countries, is taking broad, fast action to help developing countries strengthen their pandemic response. An amount of $160 billion in terms of financial support to help countries protect the poor and vulnerable, support businesses, and bolster economic recovery, including $50 billion of new IDA resources in grants or highly concessional terms has been released over the past 15 months. Through the International Development Association (IDA) of World Bank, an amount of $8.1 million was allocated to help Togo combat COVID-19 (coronavirus) and better respond to public health emergencies. To respond to the pandemic, COVID-19 Emergency Response Project was set up, to help the Government of Togo strengthen epidemiological surveillance, early detection, and confirmation of cases. The project is underway in the context of the Regional Disease Surveillance Systems Enhancement (REDISSE) Project. By building the capacity of personnel involved in the response effort, strengthening the surveillance capacity of laboratories, and facilitating the procurement of personal protective equipment and medical equipment, including resuscitation equipment the project will expand screening and patient care capacity. Heavy burdens have been placed on hospital and outpatient health services, which are on the front lines.
(Bruce Emmanuel,Assistant Researcher of CWAS,School of Management and Economics of UESTC)
Please refer to the Chinese Version published on Huanqiu.com, one of the top three rating news media in China. Huanqiu.com is a national rating on line media platform, approved by the publisher of People's Daily and the Central Internet Information Office of China. This column is to provide a platform for researchers and practitioners on West African issues.

Link:https://opinion.huanqiu.com/article/42Q6jySjpM7